Moon Mama Blog
Let’s sip tea and chat
Aloha,
I am so happy you’re here. My name is Chandra and I love LOVE educating Mothers, families, and the community on the extreme importance of taking care of our Moms during the first 42 days post birth. I have a background in Yoga, specifically prenatal and postpartum, along with using the Science of Ayurveda to heal and support the birthing parent.
In 2018 I decided I wanted to dive deep into the world of lactation. I can’t tell you how many families I worked with that were lost, unsupported, and left alone in the early Postpartum days when it came to lactation. I knew I wanted more in depth clinical knowledge to add to my background in supporting families so I dove in deep to become an IBCLC.
Jumping on a soap box… (Why does becoming an IBCLC matter!)
Because…it…is…considered the GOLD standard in the Lactation field
An IBCLC (International Board-Certified Lactation Consultant) is the highest level of lactation education one can receive, and is globally recognized as experts in the clinical management of breastfeeding and human milk feeding. We provide evidence based support for simple to complex feeding challenges for all stages of the nursing journey. We undergo rigorous training in health sciences, lactation education, and clinical experience. We are distinguished from other roles by offering comprehensive, qualified care.
Jumping off…
So long story short! An IBCLC has dedicated 1,000’s of hours to be experts at educating, and supporting families. So yes, it matters, and we CARE a lot in supporting Your journey in infant feeding.
Support & Education
That’s why I am here, my life's work is to educate, and support You! I want to be your friend, your village, and someone you can rely on during this short window of time.
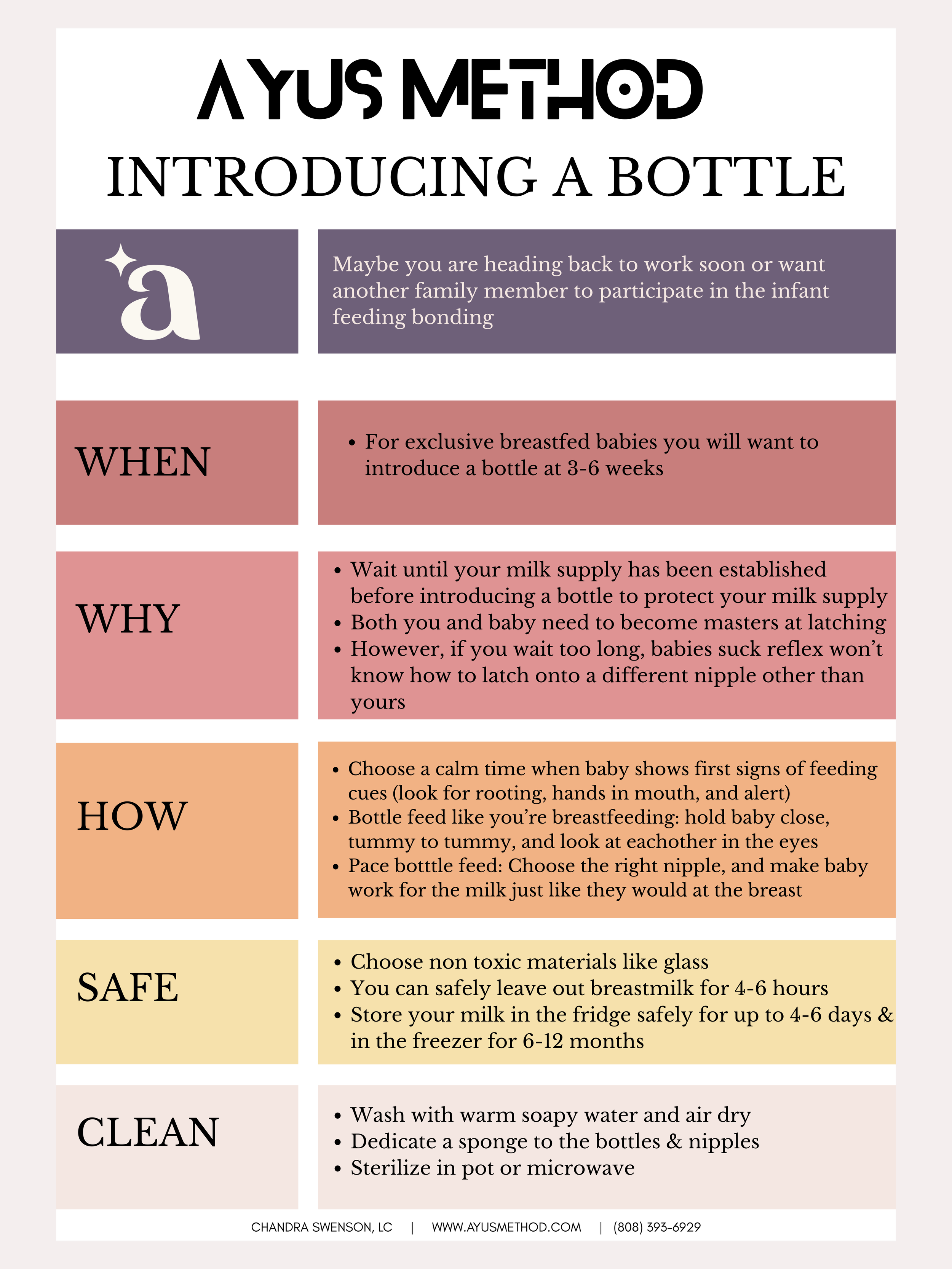
Bottles…
Many parents wonder when to introduce a bottle to their infant. Timing depends on feeding goals, milk source, and the baby's readiness. Below are clear, practical guidelines to help you decide.
WHEN TO INTRODUCE A BOTTLE
Introducing a bottle to your baby is a personal decision that depends on feeding method, goals, and family needs. Here are practical guidelines to help you choose the right timing and approach.
When to consider introducing a bottle
If you plan to breastfeed exclusively and return to work or need others to feed the baby, introduce a bottle between 3–6 weeks of age. Many parents find 3–4 weeks works well: breastfeeding is usually established, and the baby is more adaptable to a bottle.
If you’re pumping and giving expressed milk, you can start bottles as early as the first few weeks if breastfeeding is not your priority, or sooner if the infant is bottle-fed from birth.
Waiting until breastfeeding is well established (often around 3–6 weeks) reduces the chance a baby will prefer a bottle.
If medical or feeding issues require supplementation, introduce a bottle as soon as necessary. Work with your lactation consultant to protect supply and technique.
Signs your baby is ready for a bottle
Good latch and effective breastfeeding (consistent weight gain, audible swallowing, satisfied between feeds).
Calm, developed sucking coordination (usually around several weeks old).
Interest in feeding from others or readiness to accept a different feeding rhythm.
How to introduce the bottle
Use paced bottle feeding to mirror breastfeeding rhythms: hold baby upright, tilt the bottle to keep the nipple full of milk, allow pauses, and let the baby set the pace.
Offer the bottle when baby is calm and mildly hungry—not frantic. Try between the first signs of hunger and before full-blown crying.
Have someone else offer the bottle at first if the baby strongly prefers nursing to comfort from you.
Try different nipple shapes and flow rates. Start with a slow-flow nipple to mimic breastfeeding. Faster flows may cause gulping, gas, or refusal.
Warm the milk to close to body temperature if your baby prefers warmth. Test on your wrist before offering.
Offer small amounts initially to reduce waste and let baby adjust.
Protecting breastfeeding while introducing bottles
Continue breastfeeding frequently, especially daytime feeds, to maintain supply.
Pump after or between breastfeeding sessions to preserve milk supply if you’re replacing some feeds with bottles.
Avoid long stretches without breastfeeding in the early weeks if your goal is exclusive breastfeeding.
Seek support from a lactation consultant if you notice decreased supply, pain, or significant refusal.
Troubleshooting common issues
Bottle refusal: try different nipples, have someone else offer, wait and try later, or offer while baby is drowsy.
Preference for bottle: slow the bottle flow, use paced feeding, and increase breastfeeding opportunities.
Supply concerns: pump after bottle feeds, increase breastfeeding frequency, and consult a lactation professional.
Special circumstances
Premature or medically fragile infants: follow hospital and specialist guidance—bottle introduction timing may differ.
Adoptive parents or parents using donor milk: start according to feeding plan and the baby’s cues; a slow-flow bottle can work from early on.
Combination feeding: introduce bottles as needed but monitor supply and baby’s cues to maintain desired breastfeeding level.